How Greenville Family Medicine Improved Rural Healthcare with Remote Patient Monitoring and Chronic Care Management

Author
Digital health marketing professional with over 10 years of experience bridging clinical and wellness spaces by leveraging innovative technologies, behavioral change programs, and strategic digital marketing.
Rural clinics often face unique challenges in providing consistent, comprehensive care for patients with chronic conditions. Greenville Family Medicine, a community-focused clinic, was looking for ways to enhance patient engagement, improve outcomes, and streamline care delivery despite limited resources. By partnering with KangarooHealth, the clinic implemented Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) programs tailored to the needs of its patients, creating a connected care model that extends the reach of its clinical team and strengthens support for patients across the Greenville area.
KangarooHealth’s integrated approach to Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) is helping clinics deliver more responsive, coordinated care to patients with complex, chronic conditions. This case study highlights how one rural clinic leveraged the platform to strengthen care delivery for medically vulnerable patients, and the measurable impact that followed.
Chronic conditions are rarely managed in silos. For patients with high clinical complexity, the difference between crisis and stability often comes down to timely insight and reliable follow-through. This case study follows two older adults whose care journeys were transformed by the combined power of RPM and CCM, resulting in meaningful improvements in both clinical status and day-to-day confidence.
Designed for clinic leaders, providers, and care teams, this report offers a grounded look at how KangarooHealth’s technology and care coordination tools support decisions, faster interventions, and more unified care delivery. Through detailed patient journeys, platform metrics, and clinical insights, we show how a rural primary care team was able to manage risk more proactively and extend care beyond the exam room.
Together, these stories reflect a larger truth: the power of remote care lies not just in the data, but in how we translate it into timely action and better outcomes.
Clinic & Program Overview
Greenville Family Medicine is a small rural clinic located in Greenville, Illinois. Led by Dr. Hopkins, the practice serves a predominantly senior population, many of whom face multiple, ongoing chronic conditions.
In partnership with KangarooHealth, the clinic developed a data-informed workflow that transforms remote vital signs into clinical action, bridging the gap between symptom onset, provider awareness, and timely intervention.
The coordination team receives an average of 118 RPM alerts per day, 31% of which are classified as high-risk, underscoring the acuity of the patient population and the need for rapid, coordinated responses.
To address rising patient complexity and limited in-person capacity, the clinic partnered with KangarooHealth to implement RPM and CCM. These programs empower the care team to monitor patients remotely, respond quickly to health changes, and maintain consistent support between visits.
Key goals for implementing RPM and CCM included:
- Enhancing chronic condition management
- Reducing preventable hospitalizations and ED visits
- Strengthening care coordination across providers and care transitions
- Supporting timely medication adjustments through data-driven insights
The following patient stories illustrate how these programs have delivered measurable impact, for both patients and the care team.
Patient Spotlight: Opal (81, Female)
Chronic Syncope with Cardiovascular Risk
Clinical Snapshot
Opal is an 81-year-old woman with a history of recurrent, unexplained syncope and multiple high-risk cardiac conditions, including:
- Labile hypertension
- Stage 3 chronic kidney disease
- Pulmonary hypertension
- Coronary artery disease
- Aortic stenosis
Despite years of specialty care and the use of a LINQ cardiac monitor (removed in 2022), no clear cause of her syncopal episodes was identified. Sporadic home monitoring further limited clinical visibility.
“For years, challenges included finding a cause for her repeated syncope. While she would take her blood pressure and heart rate at home, she did not do it regularly or at the time of syncope.” – Dr. Hopkins
Turning Point: Fall & Hospitalization
In October 2024, Opal was admitted to Fayette County Hospital following a fall caused by a syncopal event. She had been experiencing lightheadedness but hadn’t alerted her care team. On admission, she was found to be severely hypotensive. After discharge, her medications were adjusted, and RPM was initiated during her follow-up visit on October 21, 2024.
RPM Enrollment & Early Impact
- Device Delivery: October 22, 2024
- Total BP Readings Submitted: 456
- Engagement: 5–7 readings most weeks, with just one brief gap
- First Critical Alert: Within 3 weeks, RPM flagged a dangerously high BP reading that prompted same-day clinical intervention
Consistent monitoring enabled early detection of blood pressure fluctuations, allowing the care team to respond quickly. Over time, RPM data directly informed five or more therapeutic changes, leading to reduced variability, improved stability, and fewer symptoms. In-office visits and remote medication adjustments were tailored based on ongoing RPM trends, helping to prevent further syncopal episodes and optimize long-term management.
Vital Trends & Clinical Insights
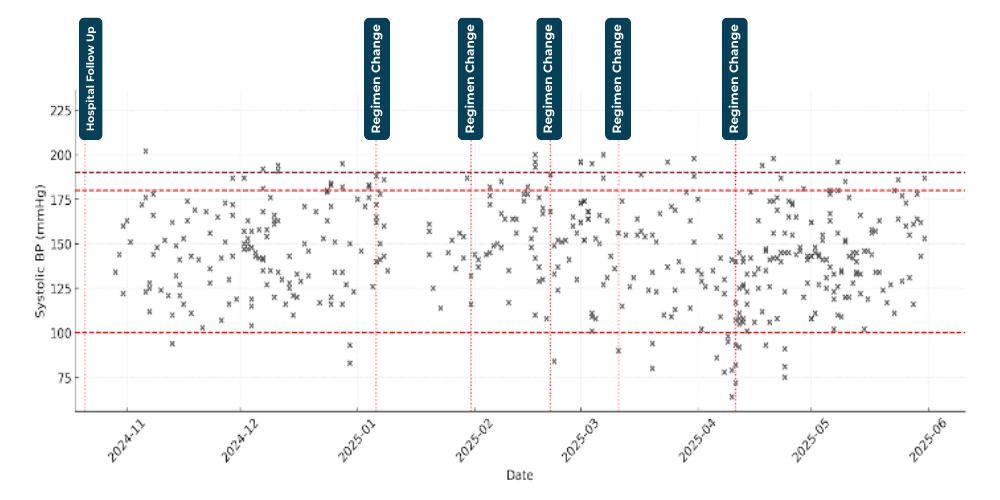
(Figure 1) Systolic blood pressure with layered regimen changes.
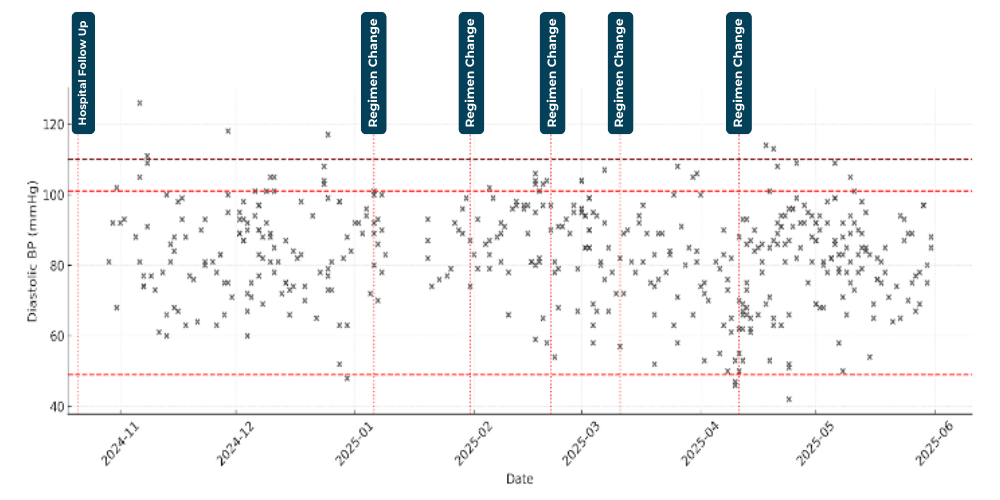
(Figure 1.1) Diastolic blood pressure layered with regimen changes.
Blood Pressure Trends & Therapeutic Response
Opal’s systolic and diastolic blood pressure readings demonstrated consistent daily variability, a pattern that posed ongoing risk without regular oversight. Systolic values, in particular, showed more pronounced fluctuations than diastolic, making it harder to establish a stable baseline.
By layering interventions on top of these trends, the care team was able to identify correlations between medication changes and shifts in blood pressure control. Over time, these targeted adjustments contributed to reduced variability, fewer high-risk alerts, and improved overall stability.
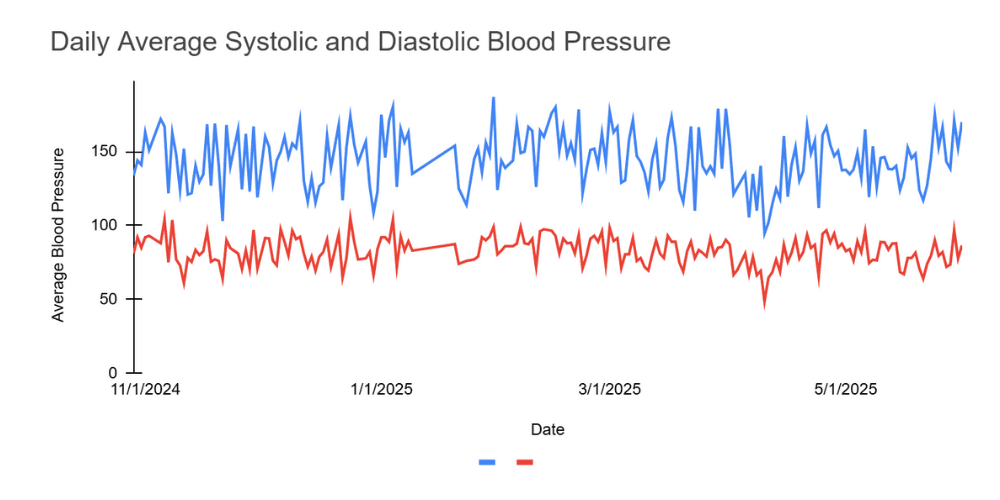
(Figure 1.2) Daily average systolic and diastolic blood pressure
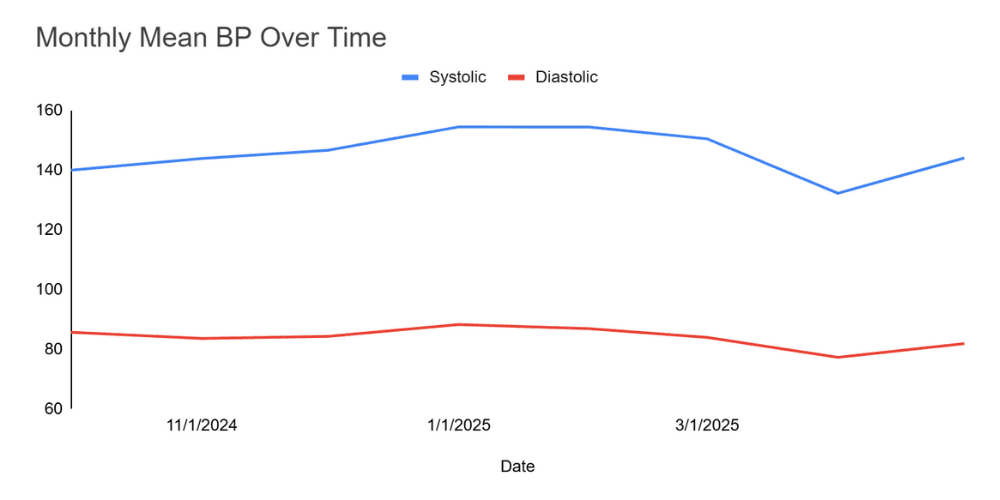
(Figure 1.3) Monthly mean blood pressure over time
Opal’s systolic and diastolic blood pressure readings demonstrate consistent daily variability; a pattern that posed ongoing risk without regular oversight. Systolic values, in particular, showed more pronounced fluctuations than diastolic, making it harder to establish a stable baseline.
By layering interventions on top of these trends, the care team was able to identify correlations between medication changes and shifts in blood pressure control. Over time, these targeted adjustments contributed to reduced variability, fewer high-risk alerts, and improved overall stability.
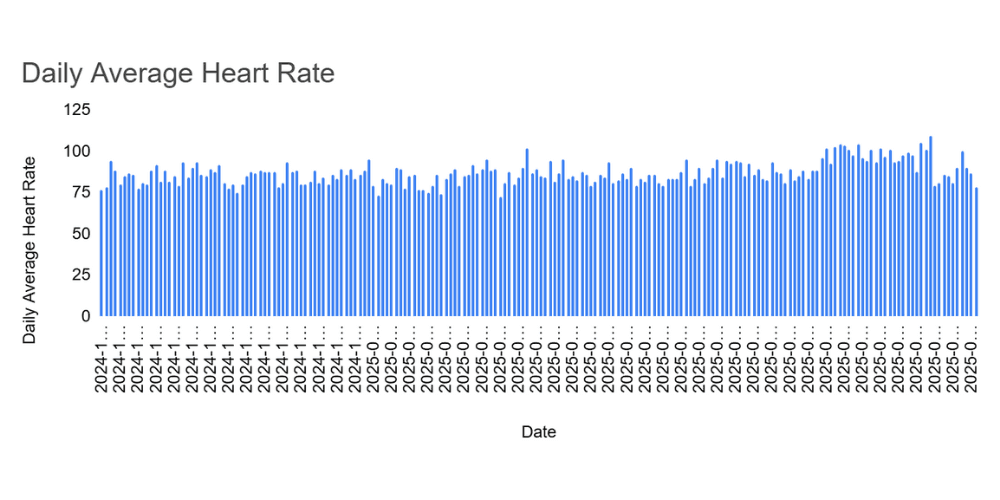
(Figure 1.4) Patient's daily heart rate
Clinical Escalation & Diagnostic Breakthrough
While RPM enabled real-time monitoring and trend identification, it also played a critical role in triggering escalation pathways, ultimately uncovering a significant underlying condition that had gone undiagnosed for years.
In April 2025, persistent and unexplained blood pressure variability prompted the care team to pursue further diagnostic evaluation. As a result:
- Findings: Renal artery stenosis and atherosclerotic aortic disease
- Follow-up: Referral to a new cardiology group, leading to cardiac catheterization in May 2025
- Outcome: Diagnosis of severe multivessel coronary artery disease (CAD), moderate right coronary disease, and aortic stenosis. The patient was managed medically, avoiding surgical intervention.
Between October 2024 and May 2025, the RPM platform flagged 56 blood pressure alerts, 37 high-priority, and 19 emergency. Importantly:
- 100% of these alerts were acknowledged with documented contact, demonstrating strong clinical follow-through
- 32% of high-priority and 26% of emergency alerts resulted in documented clinical interventions, including medication changes, referrals, or evaluations
Though not every alert necessitated a change in care, the cumulative visibility and timely outreach provided the clinical insight needed to connect the dots.
After years of diagnostic uncertainty, remote monitoring delivered the breakthrough, transforming daily vitals into actionable insight and changing the trajectory of Opal’s care.
Coordinated Monitoring in Action
RPM & CCM Engagement Overview
The following tables provide a detailed view of Opal’s care coordination through both Remote Patient Monitoring (RPM) and Chronic Care Management (CCM). Together, these programs offered continuous oversight, connecting real-time physiologic data with clinical decision-making and timely outreach.
RPM data not only surfaced critical trends but also prompted time-sensitive responses, many of which were documented with specific actions, follow-up notes, or medication changes. In parallel, CCM engagement helped maintain continuity between visits, reinforcing adherence and supporting the patient through ongoing education and check-ins.
This integrated approach ensured that no alert went unnoticed and that Opal received consistent, proactive support throughout her care journey.
Summary of RPM Alerts
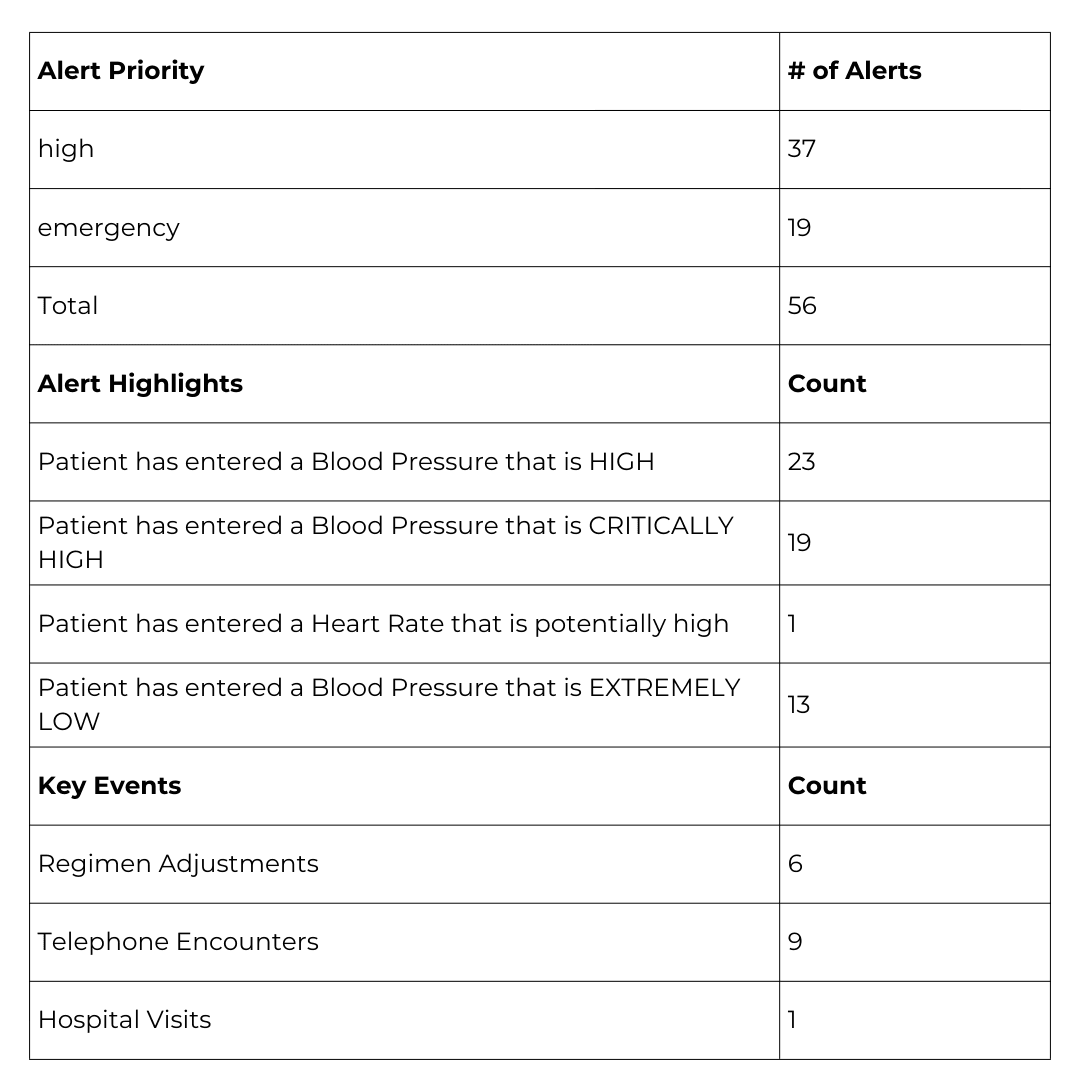
(Figure 1.5) Summary of RPM alerts gives a breakdown of the patient's alert activity.
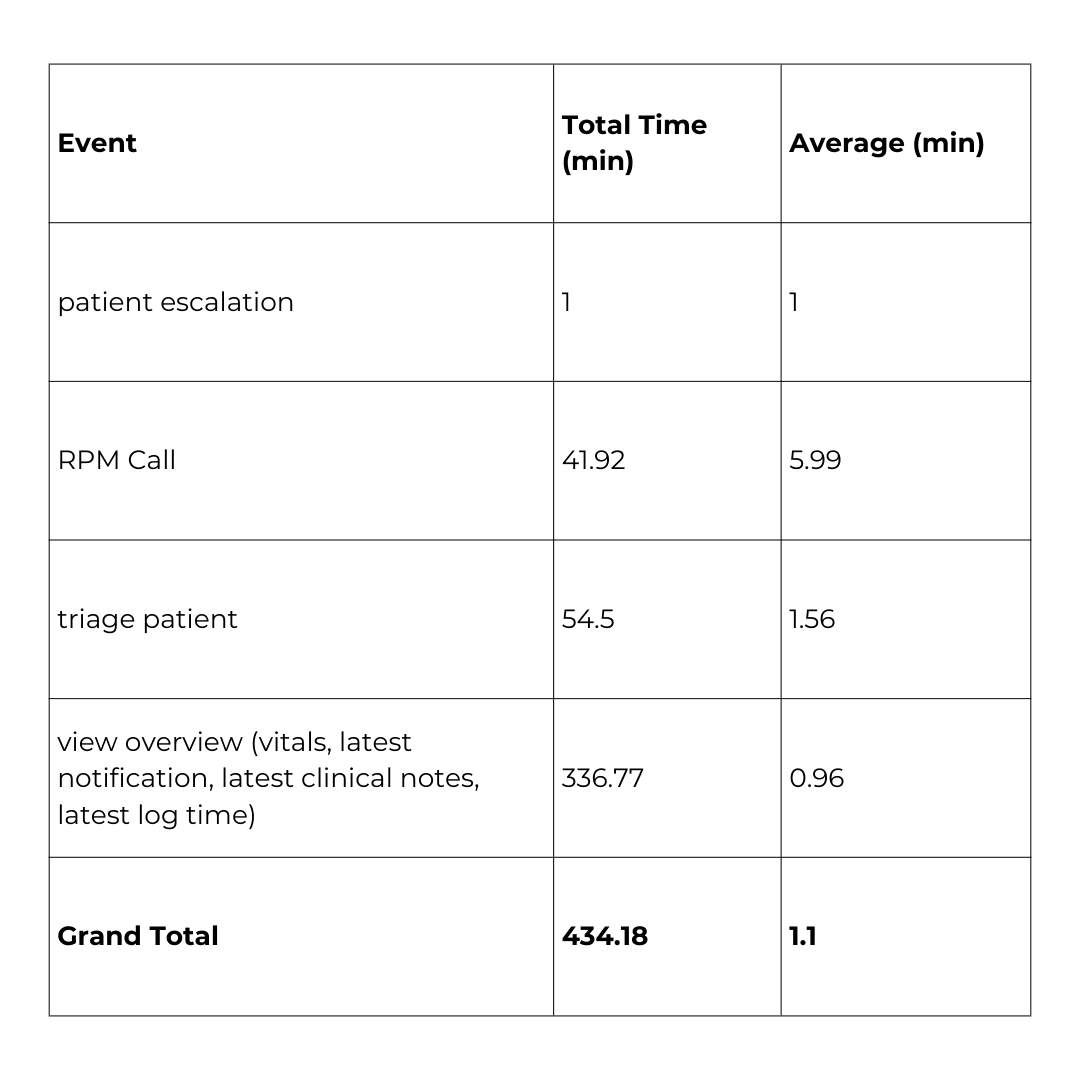
(Figure 1.6) Summary of RPM Monitoring

(Figure 1.7) Summary of CCM monitoring time
Risk Reduction & Recovery
Following her enrollment in RPM, Opal demonstrated strong engagement, consistently submitting daily readings. Between November 2024 and May 2025, she transmitted over 450 blood pressure measurements, enabling continuous clinical oversight and early pattern recognition. During this period:
- No falls or emergency department visits were recorded
- All episodes of dizziness or symptomatic hypertension were addressed through same-day outreach or timely follow-ups
- RPM data informed at least five therapeutic changes, leading to improved blood pressure control and likely reducing her risk of acute decompensation.
Provider Insight
“Undoubtedly, the intensive monitoring performed through RPM with KangarooHealth has provided real-time data for clinical decision-making in a patient with a complicated medical history. Early detection, timely communication, and rapid interventions likely prevented further falls, ER visits, and morbidity.” - Dr. Hopkins
In the Patient’s Words
“I feel like there have been several times when I’ve felt dizzy, and Kangaroo Health makes me more aware that my blood pressure could be a problem. I would have passed out several times had they not called me.”
Takeaway
Opal’s journey reflects the power of continuous monitoring to shift care from reactive to responsive, and from uncertain to informed. With RPM, her care team was able to detect early warning signs, intervene quickly, and uncover previously undiagnosed cardiovascular disease through trend-based insights.
Instead of repeated falls and unexplained symptoms, Opal now experiences improved stability, greater clinical confidence, and a more connected care experience. In a medically frail patient with a history of syncope, RPM may have played a decisive role in preventing serious harm, or worse.
Her case illustrates the diagnostic value of remote monitoring in complex patients and reinforces its role as a proactive tool for risk reduction, earlier diagnosis, and safer care at home.
Patient Spotlight: James (82, Male)
Managing Multi-System Illness with RPM + CCM
Clinical Snapshot
James is an 82-year-old man living with multiple severe and progressive conditions, including:
- Hypertension
- Parkinson’s disease
- Brain tumor
- Prostate cancer
- Obstructive sleep apnea
- Malignant melanoma
Over the past year, his condition grew increasingly unstable. He experienced multiple hospitalizations, sometimes twice in a single month, due to recurrent pneumonia, pleural effusions, and sepsis following acute cholecystitis.
“James was on CCM services for years past; however, the RPM services to monitor his BP, heart rate, pulse oximetry, and weight has provided real-time information about this critically ill patient.“ - Dr. Hopkins.
Clinical Challenges
Multiple, compounding issues complicated James’s care:
- Chronic fatigue and bradycardia, leading to pacemaker placement (later removed due to infection)
- Recurrent fluid buildup in the chest requiring repeated hospitalizations
- +18 lbs in weight gain from fluid retention and worsening symptoms
- New diagnosis: Heart Failure with Preserved Ejection Fraction (HFpEF)
The Role of RPM + CCM in James’s Care
While James had long been enrolled in Chronic Care Management (CCM), his increasing instability required a more dynamic layer of oversight. Remote Patient Monitoring (RPM) was introduced to support early detection and enable faster clinical response.
Through KangarooHealth’s platform, the care team began monitoring:
- Blood pressure
- Heart rate
- Weight
- Oxygen saturation (SpO₂)
Together, RPM and CCM provided a real-time view of James’s health trajectory, capturing the subtle signs of decompensation before they became emergencies. This integrated approach supported earlier interventions, better risk management, and more coordinated care for a highly complex patient.
Alert Volume & Clinical Actions
Among the 250+ alerts within the RPM program, the following are some of the most frequently occurring alerts for James. Each alert was managed according to tailored care plans and clinic-specific escalation protocols, all customized to James’s unique clinical needs and guided by physician recommendations.
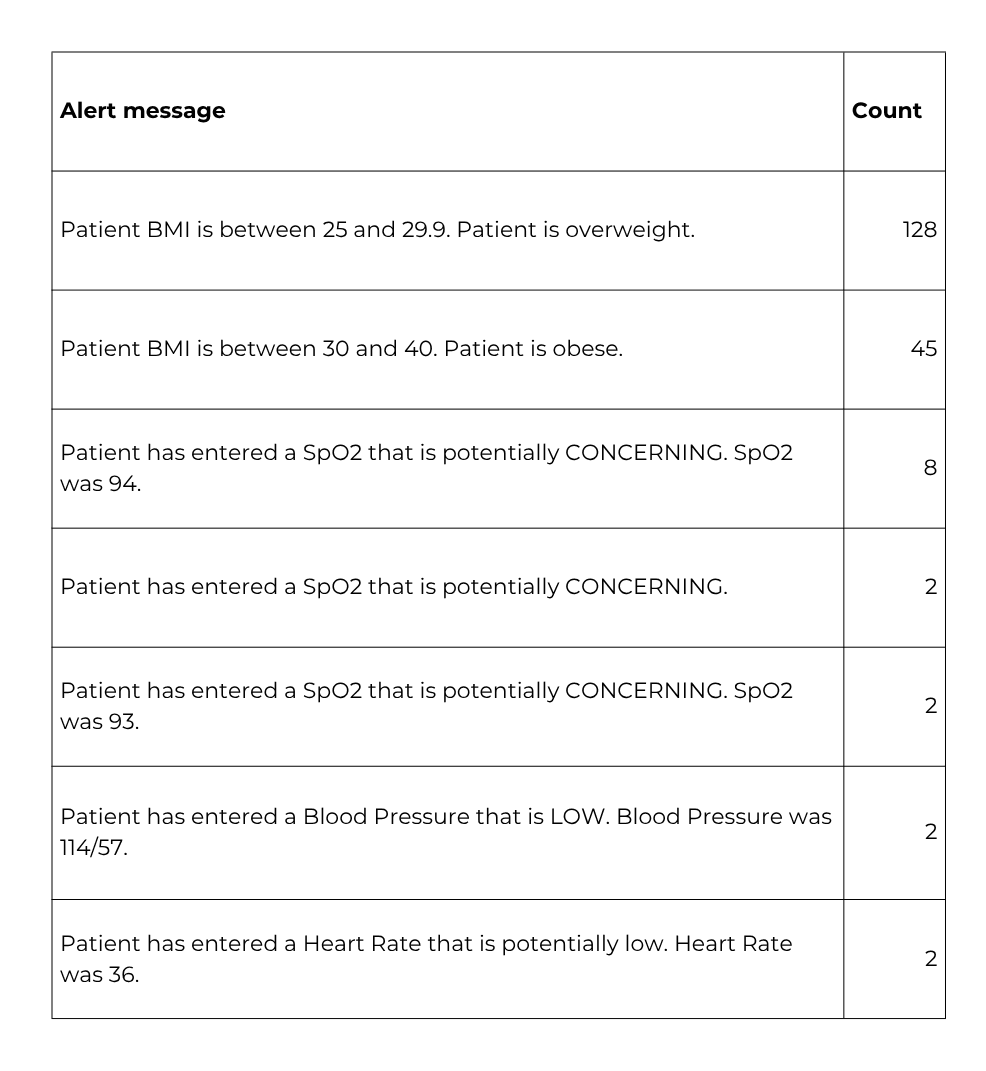
Figure 2
Alert Distribution
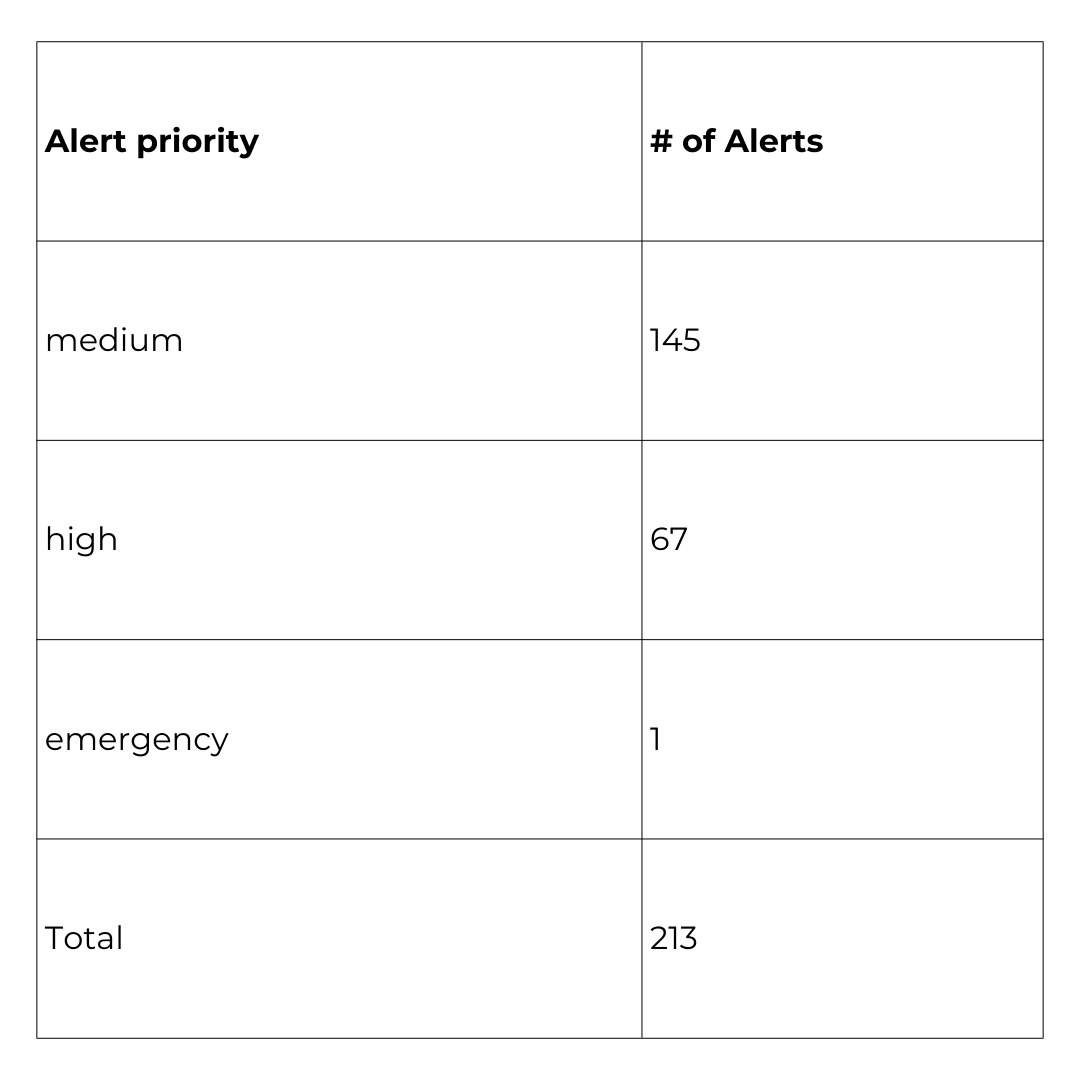
(Figure 2.1)
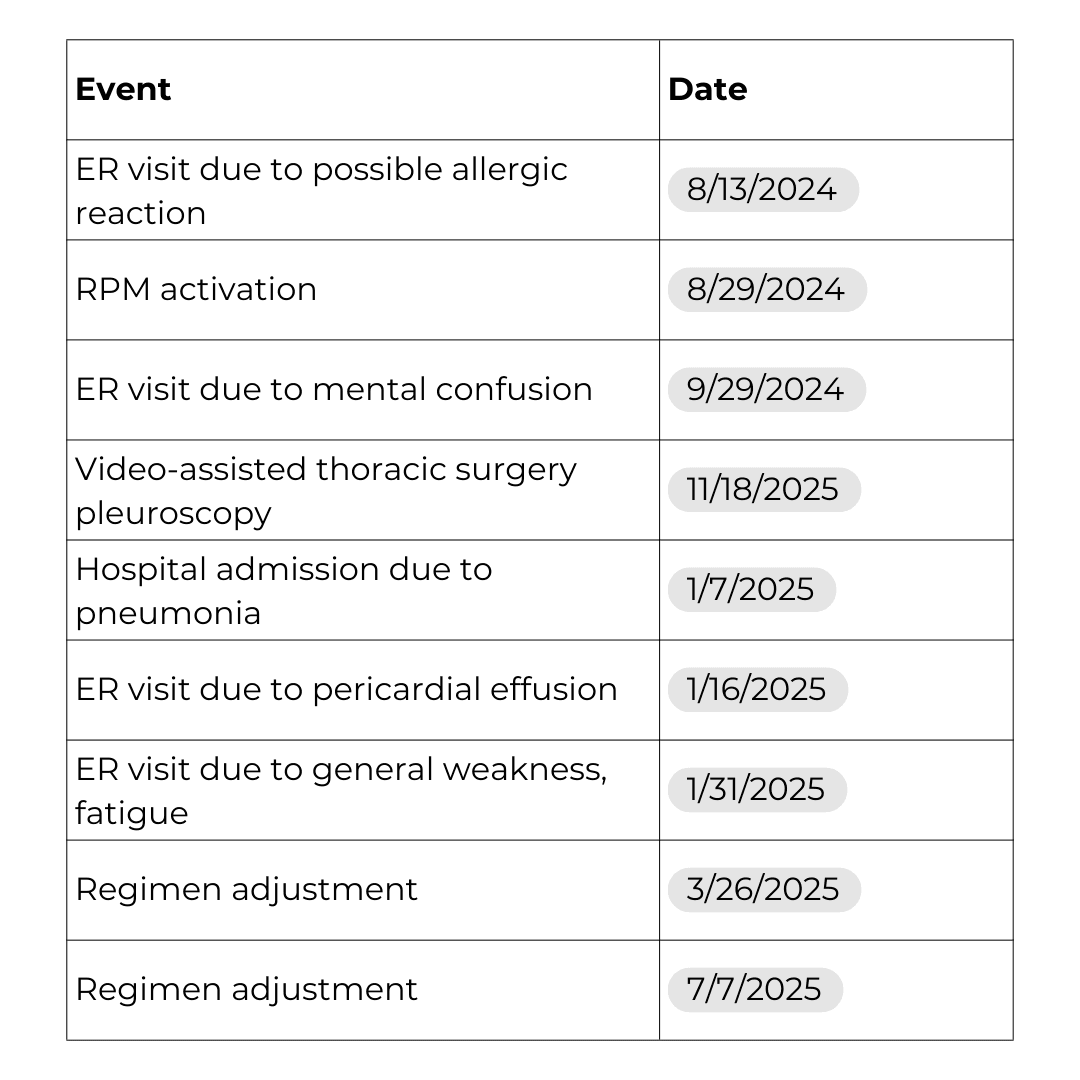
Key Events
| Column 1 | Column 2 | Column 3 |
|---|---|---|
Hospital Admissions | 5 | |
Regimen Adjustment | 2 | |
Procedure | 1 | |
Follow-Ups and Encounters | 20 |
(Figure 2.2)
Notable Interventions
Monitoring Trends & Key Insights
James’s RPM data revealed early signs of fluid overload well before symptoms became clinically apparent. This timely insight allowed the care team to make medication adjustments aligned with established protocols and his personalized care plan.
Key observations include:
- September 2024: Rapid weight gain of 4 pounds over two days
- April–June 2025: Significant weight increase totaling 18 pounds
These trends preceded James’s formal diagnosis of heart failure with preserved ejection fraction (HFpEF) and guided appropriate therapeutic interventions. By detecting these changes remotely, the team was able to act sooner, well ahead of scheduled office visits, helping to stabilize his condition and reduce the risk of acute exacerbations.
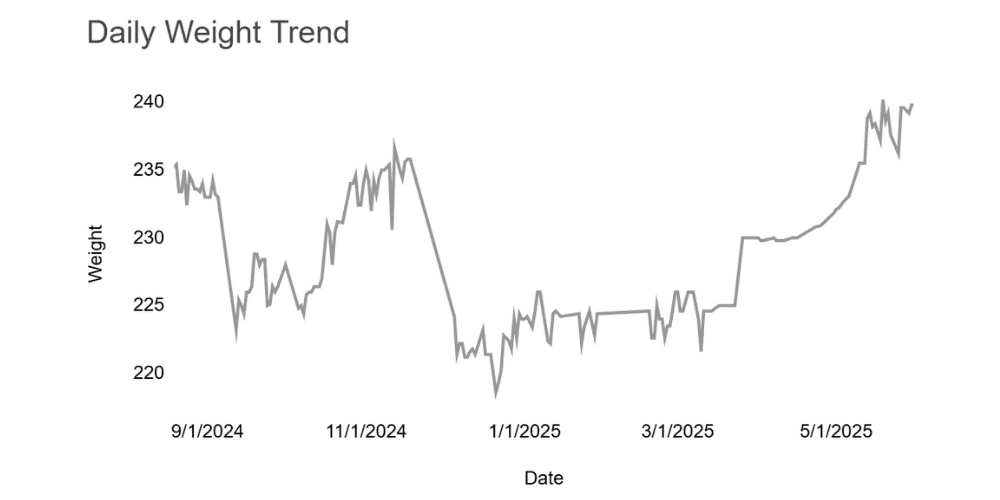
(Figure 2.4)
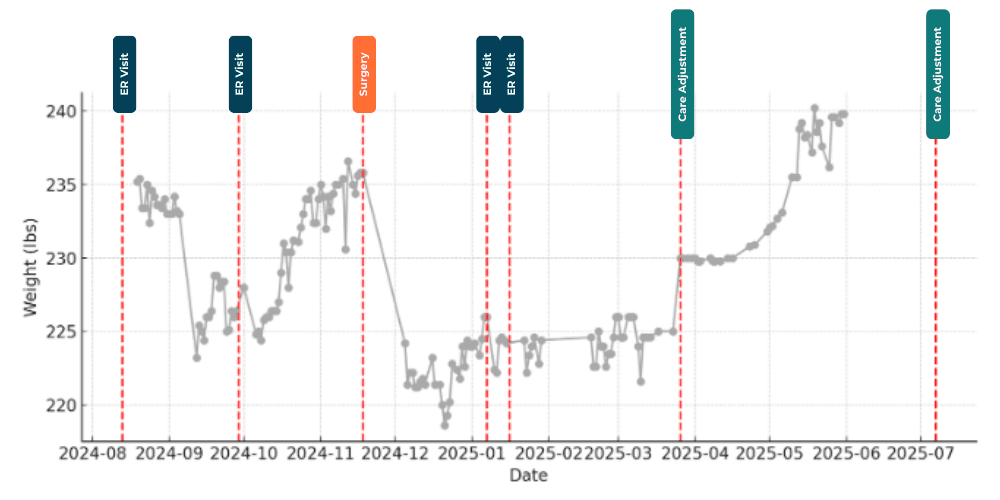
(Figure 2.5) Weight over time layered with notable clinical events.
The average weight trend over time showed notable fluctuations corresponding with key clinical events and interventions.
- August to October 2024: James’s weight started near 233 lbs in August, dipped slightly in early September, then gradually rose to about 234 lbs by late October.
- November to December 2024: A significant weight drop occurred, falling from roughly 235 lbs to 222 lbs by year-end. This decrease coincided with his diagnosis of pleural effusion and the pleuroscopy procedure performed in November.
- January to May 2025: Beginning in January, weight steadily increased, from approximately 224 lbs to nearly 240 lbs by May. This upward trend aligned with a more sedentary lifestyle, ongoing edema, and likely fluid retention.
Remote monitoring staff identified these changes promptly, notifying James’s provider, which led to a medication regimen adjustment in March 2025.
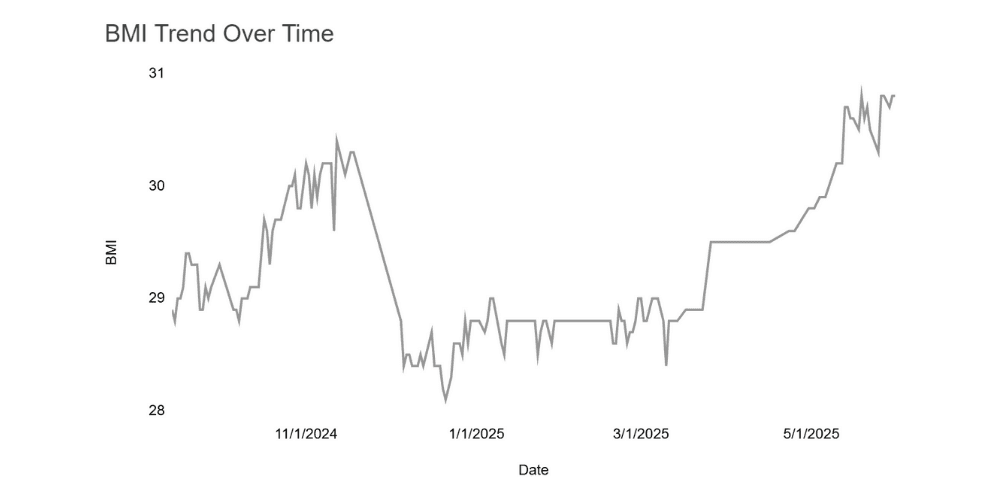
(Figure 2.6) BMI trend over time.
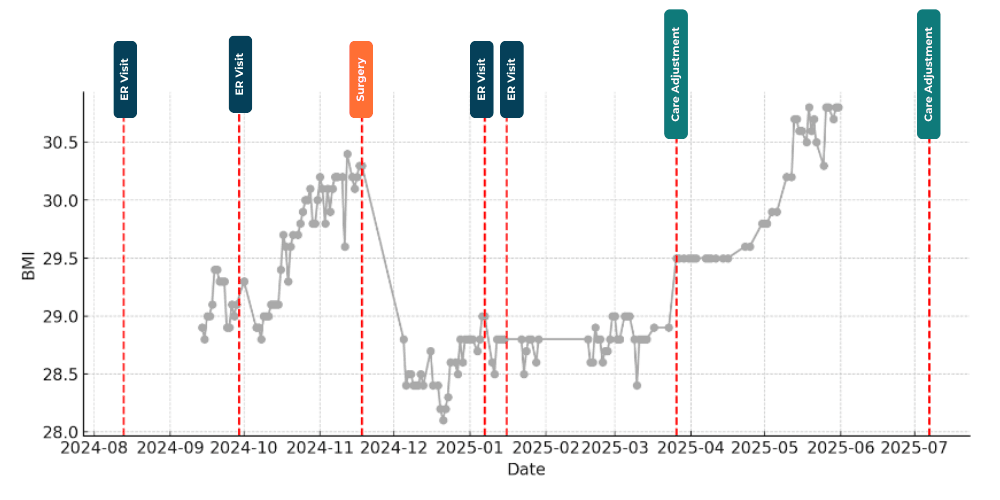
(Figure 2.7) Monthly BMI average.
The BMI trends further reflected James’s evolving clinical status over time.
- In 2024, the highest average BMI was recorded in November (30.12), followed by a notable decrease to 28.49 in December.
- In 2025, BMI steadily increased from 28.76 in January to 30.43 by May.
This upward trend coincided with James’s sedentary lifestyle, ongoing edema, and likely fluid retention.
The remote monitoring team quickly identified these changes and alerted the treating provider, prompting medication adjustments in March 2025.
Supporting data, including blood pressure, heart rate, and oxygen saturation readings, corroborated these findings and guided ongoing clinical decision-making.
(Figure 2.8)
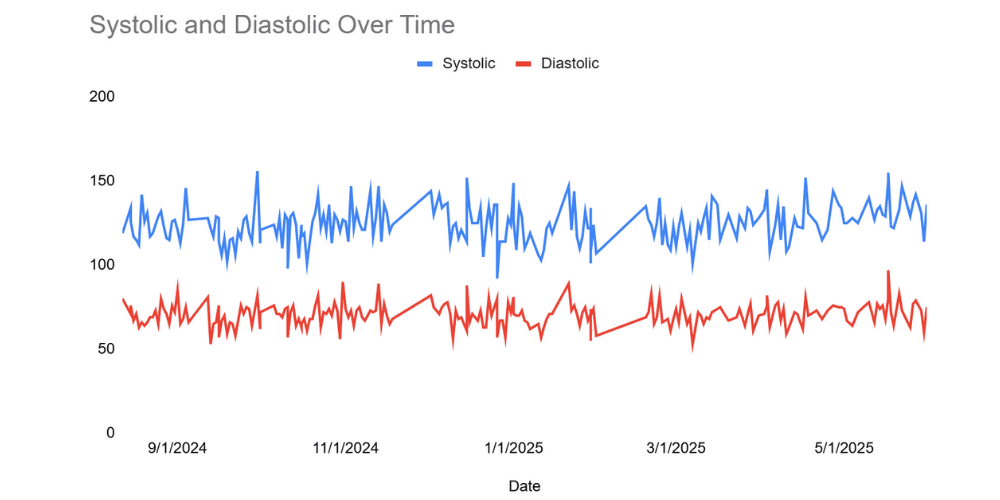
Overall Blood Pressure Levels
James’s average systolic blood pressure was approximately 124.35 mmHg, with individual readings ranging from 92 mmHg to 156 mmHg. Most systolic values clustered between 116 mmHg and 131 mmHg.
His average diastolic blood pressure was about 70.46 mmHg, typically ranging from 53 mmHg to 97 mmHg, with the majority of readings falling between 66 mmHg and 74.75 mmHg.
These values reflect generally stable blood pressure control, with occasional fluctuations captured by the RPM system that informed timely clinical interventions.
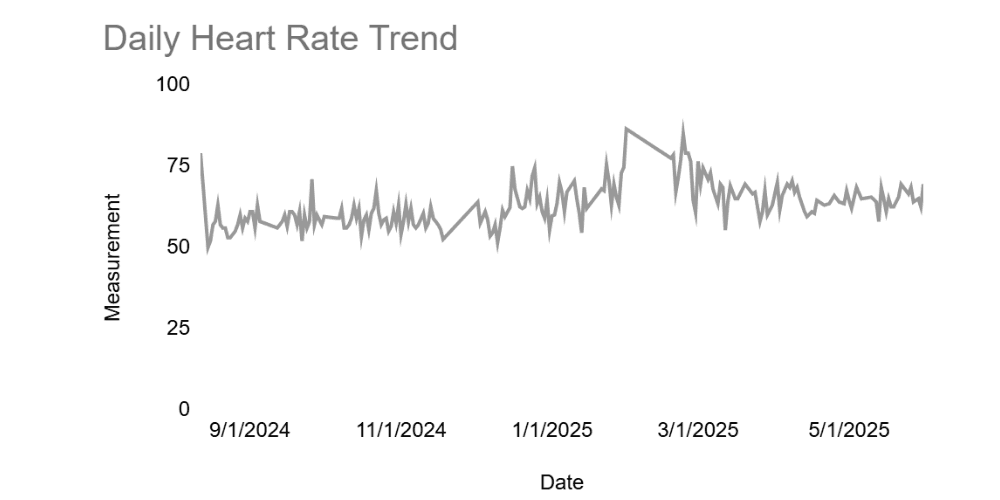
(Figure 2.9) Heart rate trend.
Heart Rate Overview (August 2024 – May 2025)
James’s heart rate data revealed an average of approximately 63.74 beats per minute (bpm) across all measurements, with values ranging from a low of 35 bpm to a high of 88 bpm.
Key observations include:
- Most readings cluster around the average of 63.74 bpm.
- Daily and monthly trends show fluctuations, with a general upward trend in heart rate from late 2024 into early 2025.
- The distribution of heart rate measurements is approximately normal but slightly skewed, with a prominent peak in the 60–70 bpm range.
Lower and higher extremes, such as 35–40 bpm and 85–90 bpm, occurred less frequently, indicating these are atypical readings.
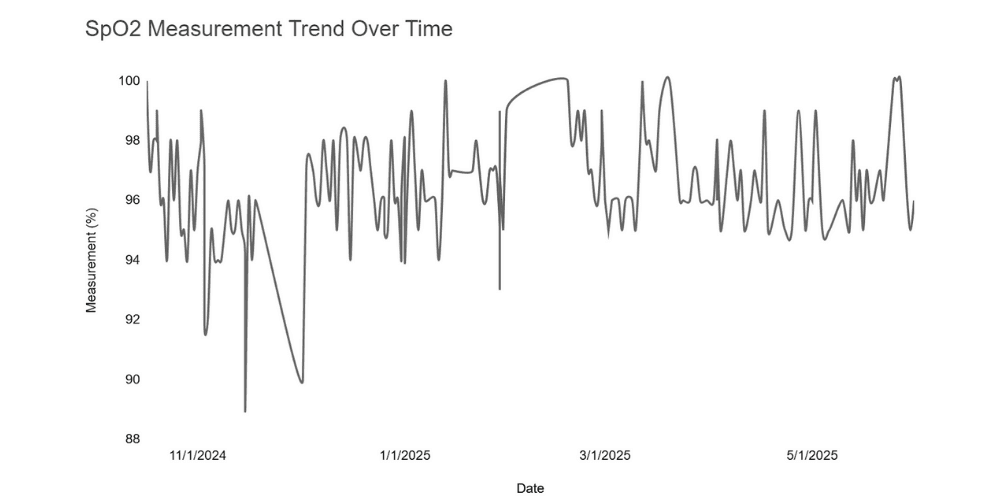
(Figure 2.10)
SpO₂ levels remained stable with a mean of 96.4%, showing occasional dips as low as 89%. A gradual upward trend from October 2024 to May 2025 reflects overall respiratory improvement.
CCM Coordination: Bridging Fragmented Care
James was under the care of multiple specialists across different hospital systems. Chronic Care Management (CCM) monthly summaries played a vital role by providing:
- A consolidated view of his clinical course
- A reliable communication channel back to primary care
- Better insight into new diagnoses and treatment changes
“One of the most hopeful things about chronic care management services in a patient with Jim's complexity is the summation of information on a monthly basis that highlights the changes since he was last in the office.” - Dr. Hopkins
Takeaway: Clinical Stability Through Coordinated Monitoring
James’s experience highlights how continuous monitoring combined with coordinated care can improve outcomes for patients with complex, fluctuating health conditions.
With multiple chronic illnesses and frequent hospitalizations, his health status changed often, challenges that could not be managed through office visits alone.
Remote Patient Monitoring (RPM) offered daily visibility into key metrics, weight, blood pressure, heart rate, and oxygen saturation, revealing early signs of decline and enabling timely medication adjustments and interventions.
Meanwhile, CCM ensured a consistent connection between visits. Monthly outreach by the care coordinator captured updates on symptoms, side effects, and daily challenges directly from James. This ongoing communication gave his primary care provider clear, up-to-date insights to support clinical decisions, reinforce care goals, and prompt early action when needed.
By combining RPM and CCM, James’s care team detected issues sooner and maintained a more consistent level of care. This connected approach provided James with greater stability during a vulnerable period and enabled providers to respond swiftly and effectively.
“The RPM services for this individual were critical because he was so ill for so many months that the quick interpretation of data that had changed, such as his weight, allowed for rapid changes in therapy to help speed recovery and reduce further complications.”- Dr. Hopkins
Conclusion & Next Steps
The experiences of James and Opal showcase the powerful, multifaceted impact of integrating Remote Patient Monitoring (RPM) and Chronic Care Management (CCM). From enabling rapid responses to fluid overload and blood pressure instability to uncovering previously hidden diagnoses like renal artery stenosis, these programs provide timely insights that translate into meaningful clinical action and improved outcomes.
“From a sudden spike in vitals to a subtle change in patient-reported outcomes, we at KangarooHealth make sure providers get the right information at the right time. Because the future of care isn’t about collecting more data. It’s about acting on the right data.” - Dr. Kang CEO & Founder of KangarooHealth
Both patients benefited from earlier identification of clinical issues and more timely medication adjustments through continuous monitoring. The integration of RPM and CCM strengthened communication channels, surfaced critical changes in health status, and supported informed decision-making between visits. Notably, James and Opal both reported feeling more connected to their care teams and more confident managing their health.
As healthcare continues to evolve, case studies like these provide more than validation; they offer a blueprint for expanding virtual care programs that are clinically effective, operationally sustainable, and deeply human. The partnership with Greenville Family Medicine reflects how technology and clinical collaboration can come together to extend care and create lasting impact for patients in rural communities.

Sesily Maness
AuthorDigital health marketing professional with over 10 years of experience bridging clinical and wellness spaces by leveraging innovative technologies, behavioral change programs, and strategic digital marketing.