6 Benefits of Remote Patient Monitoring in Modern Healthcare

Author
Digital health marketing professional with over 10 years of experience bridging clinical and wellness spaces by leveraging innovative technologies, behavioral change programs, and strategic digital marketing.
The RPM (Remote Patient Monitoring) market is projected to record a compound annual growth rate (CAGR) of 19.8% in the medium- to long-term. What's driving such broad adoption? One explanation is the increasingly undeniable benefits of remote patient monitoring. RPM creates an enticing win-win scenario for providers and patients. Patients get high-quality, cost-competitive care, and their providers benefit from higher operational efficiency and improved quality metrics like lower hospital readmission rates. Ready to unlock these benefits and more for your practice? See how KangarooHealth's comprehensive RPM solutions can help you unlock new opportunities without disrupting your established workflows. We handle device procurement and distribution, patient training and education, and alerts with tailored escalation protocols to prevent provider overwhelm.
The Expanding Role of RPM in Modern Healthcare
Modern US healthcare is steadily taking a value-based approach. Focus has shifted significantly from sheer volume of health services provided to ensuring superior patient outcomes.
The core principles of value-based care are:
- Accountability and transparency
- Quality over quantity
- Focus on outcomes
- Patient centeredness
- Care coordination
- Cost effectiveness
For chronic conditions, improving care in this way requires providers to extend their reach beyond the clinic walls to serve patients in their homes. Remote patient monitoring (RPM) technology now makes this possible.
Providers are increasingly using RPM technology and services to manage conditions such as diabetes and pre-diabetes, hypertension, congestive heart failure, asthma, obesity, chronic kidney disease, and more.

Key Benefits of Remote Patient Monitoring
Remote Patient Monitoring has significantly enhanced care delivery across the board.
Let's explore some of its key benefits for providers and patients:
1. Underserved Populations Have Increased Access to Care
There exists a geographic, economic, and digital divide in healthcare access. These access problems affect patients’ ability to receive quality care and hamper adherence to recommended lifestyles and treatment plans.
For example, a study analyzing adherence to antihypertensive medication among young adults found rural residence and lower household income to be negatively associated with good adherence.
While 20% of our population lives in rural areas, only 10% of providers live there. However, RPM technology is stepping up to address some healthcare challenges rural and lower-income communities face, such as distance to care and provider shortages.
Providers can now serve these communities without requiring them to visit clinics in person, enhancing engagement and lowering costs.
2. Cost Management for Both Providers and Patients
In most cases, RPM programs will generate enough revenue to cover their own costs and report a positive return on investment (ROI). For instance, a study analyzing the financial sustainability of RPM for hypertension in the cardiology practice of a large healthcare system recorded a 22% average ROI at 55% compliance.
It's noteworthy that Medicare and many private insurers now cover RPM. With KangarooHealth, most of your patients will have $0 out-of-pocket expenses. Depending on insurance plans, however, some may have minimum financial responsibility, e.g., copays.
But when RPM reduces in-person visits, overall copays also reduce. Therefore, patients under these programs are more likely to stay on track with the care plan.

3. Reduced Hospital Readmissions and ED Visits
RPM technology enables continuous monitoring and real-time data updates. With increased visibility of patient data, providers can prevent adverse events before they happen. The result is fewer readmissions and ED visits.
Readmissions and emergency departments are enormous resource burdens for hospitals. If you make significant headway in this area, you can cut costs substantially.
A study on whether telemonitoring can reduce hospitalization and the cost of care among patients with heart failure recorded some interesting stats.
In the sample enrolled in the telemonitoring group for 24 months out of the 70-month observation period, the odds of experiencing 30-day and 90-day readmission were 44% and 38% lower, respectively. These reductions translated to an approximate 11% cost savings for the payor.
4. Enhanced Patient Engagement and Satisfaction
Patients want greater control of their healthcare journey. Remote patient monitoring tools make patients active participants in their own healthcare, greatly enhancing adherence and giving them significant personal satisfaction.
The improvements caregivers have reported on increased patient satisfaction due to RPM programs are staggering. For instance, a study evaluating patient satisfaction with an RPM program for acute and chronic condition management saw patient satisfaction scores of 93.58%.
Notably, nearly all patients who go through an RPM program like it so much that they would recommend it to other patients with similar conditions. The number was 92.76% in this study.

5. Better Data Management and Data-Driven Healthcare
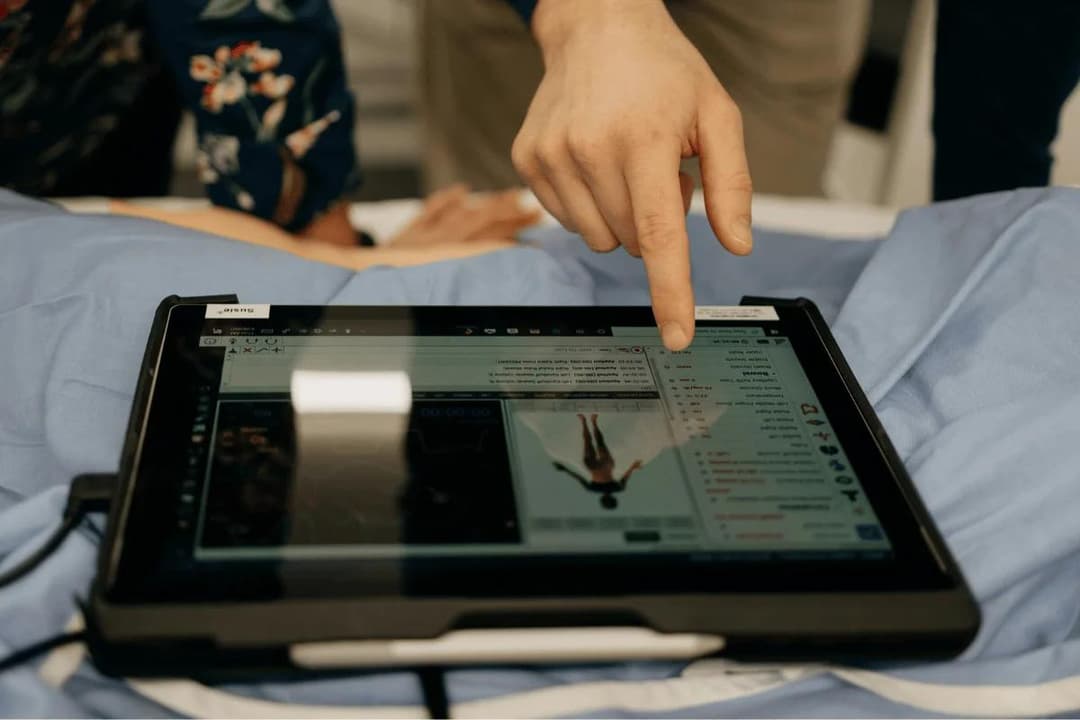
RPM technology solutions enable continuous, real-time data collection and transmission, as well as automated data processing and analysis. The platforms also allow you to centralize data from several devices or sources in one place.
The improved data management capabilities eliminate data silos that prevent care staff from getting a comprehensive view of a patient's condition or health trajectory. You can then provide personalized data-driven care, leading to superior outcomes.
6. Establishes a Feedback Loop for Patients
Lifestyle factors greatly influence outcomes when managing chronic conditions. However, it can be a challenge getting patients to adopt desirable lifestyles when they can't draw a direct connection between their actions and the physiological consequences.
RPM platforms and apps provide almost immediate feedback to patients - making cause and effect relationships undeniably clear.
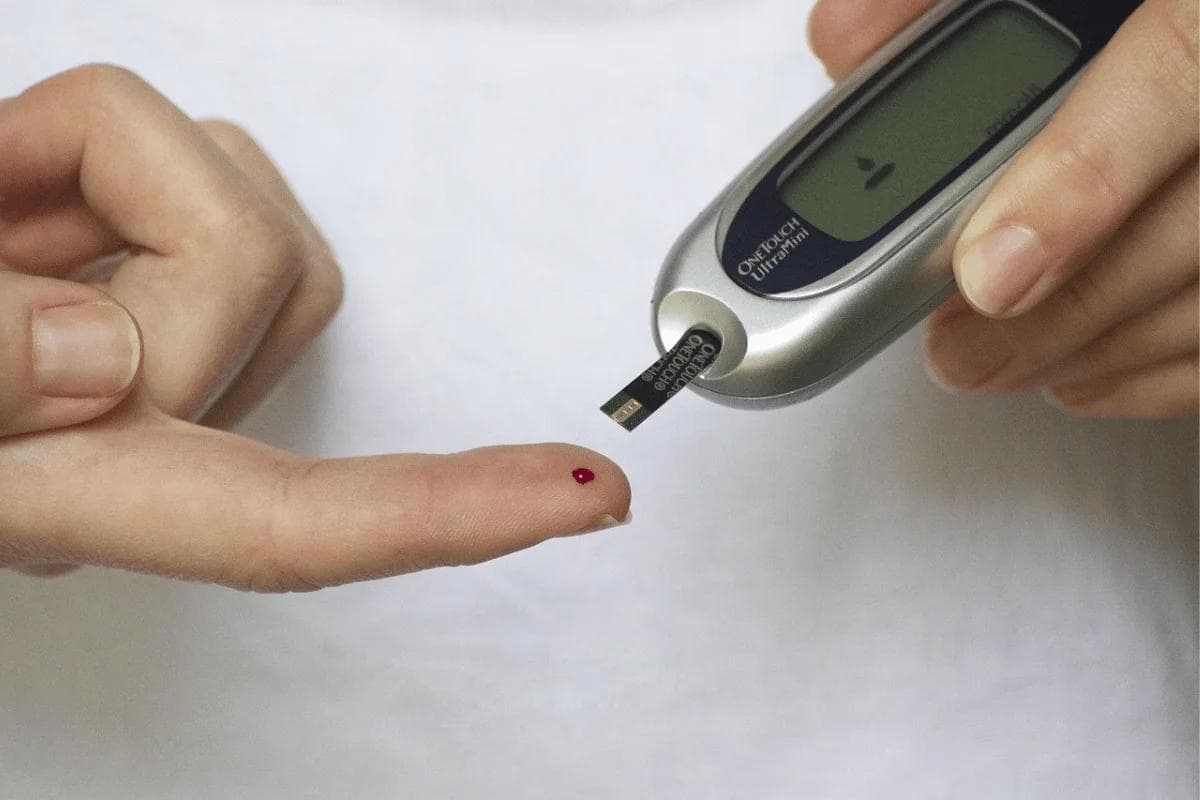
For instance, imagine a diabetes patient with a glucometer and/or continuous glucose monitor transmitting glucose level readings to an RPM app they monitor. If they eat a meal, within an hour or so, they'll see their blood sugar readings spike if it was carbohydrate- or sugar-rich.
Conversely, if they have a healthier meal, they'll see their glucose levels remain stable. Over time, the patient learns what actions serve their health goals, and they can independently make choices that lead to better outcomes in the long term.

RPM Devices: Types and Uses
Depending on the condition, you'll generally need the following RPM devices:
- Blood pressure monitors such as arm cuffs and wrist cuffs for hypertension or cardiovascular disease
- Blood glucose monitors such as glucometers and continuous glucose monitors
- Cardiac monitors for post-surgical recovery or chronic cardiac conditions
- Pulse oximeters to measure oxygen saturation in the blood
- Smart weight scales to measure and track body weight
- Spirometers for patients with lung diseases
- Smart thermometers
RPM devices primarily differ from other medical devices due to their connectivity. They collect and transmit data remotely, sometimes without patient-provided Wi-Fi, Bluetooth, or smartphones.

How Remote Patient Monitoring Enhances Outcomes
From the benefits discussed above, we’ve already established that RPM enhances healthcare outcomes by:
- Enabling personalized care at scale
- Enabling early detection and intervention
- Enhancing patient engagement and satisfaction
- Improving ongoing chronic condition management
- Giving patients visibility on how their actions affect health outcomes
- Increasing access to care for underserved and vulnerable populations
- Reducing hospitalizations and readmissions, which has an effect on cost management
Now, you might be wondering how you can set up a comprehensive RPM program to achieve these outcomes.
An effective program will generally require the following components to achieve the above outcomes:
- Robust data collection and transmission capability: You must tailor RPM devices to the patient population. For instance, rural diabetes patients will benefit from cellular-powered glucometers that don't require patient-provided internet or smartphones.
- Excellent data aggregation capabilities: Your RPM program needs a central repository. A cloud platform to aggregate, store, and standardize data is essential.
- Data analysis capabilities: The data isn't helpful if it can't give you actionable insights. Your RPM platform should be able to analyze trends, detect anomalies, and generate alerts (preferably with prioritization).
- The human and personalized touch: Even with tech involved, the human touch is essential. Continuous feedback and engagement with your care staff will help patients achieve superior outcomes.
Remote patient monitoring, therefore, enhances outcomes by providing the infrastructure to establish a continuous loop of data collection/transmission, data analysis, and timely intervention based on reliable real-time information.
KangarooHealth can help you deploy such infrastructure affordably.

How KangarooHealth Can Help You
The infrastructure required to roll out an effective RPM program is massive. Fortunately, you don't have to do everything independently. You can plug into our existing infrastructure and vendor relationships to save money and time.
With KangarooHealth, you get:
- A device-agnostic platform that integrates with several FDA-cleared devices so your patients can use tools they're already familiar with.
- Advanced analytics to generate tiered alerts so you can escalate serious complications promptly.
- A robust RPM cloud platform that's been tested in several remote patient care settings.
- Ability to seamlessly integrate with your existing Electronic Health Record (EHR).
- Help with billing, compliance, and reimbursements.
Also, we don't ensure a good experience for just you as the provider; we also improve the patient experience. Your patients will have a user-friendly service specifically designed to help them achieve superior outcomes.
Implementing RPM alone as a provider can be a significant drain on your time and resources. Using KangarooHealth saves you time and ensures you focus on what you do best - providing high-quality patient care. We'll handle device selection, procurement, and distribution as well as patient enrollment, training, and education.
Schedule a free demo with our team today, and we'll walk you through our comprehensive RPM solutions.

Common Challenges and Solutions in RPM Implementation
With great planning, your RPM program implementation will likely be a success. Some challenges are to be expected, however.
Here are some of the issues you should look out for:
- Underwhelming compliance rates: Patients may not understand how the program benefits their health, leading to low compliance. You can increase compliance by explaining the “why” behind the program and the potential benefits.
- Digital literacy problems: Many of the patients will be elderly. They may lack the digital proficiency to ensure a smooth program. Select user-friendly, simple devices and provide extensive device training.
- Interoperability problems: RPM devices and platforms often collect and aggregate data in proprietary formats, complicating interoperability. You want to use a device-agnostic RPM platform that can seamlessly integrate with services and devices from other companies.
Also, the success of an RPM program depends on seamless connectivity. The vendor should guarantee consistent data transmission, especially if you are in a rural area without reliable internet services.
Frequently Asked Questions (FAQs)
Looking for more information about remote patient monitoring? Let's explore some of the common questions we get:
How Is Remote Patient Monitoring Different From Telehealth?
Telehealth is the umbrella term for delivering healthcare services remotely with the help of various digital technologies.
RPM is a subset of telehealth, focusing on collecting and transmitting physiological data from the patient's home to their provider.
What Data Is Collected Through RPM Systems?
The data collected will depend on the condition you want to monitor and the devices you employ. You'll generally need to track:
- Physiological data: Includes weight, blood glucose levels, and respiratory rate.
- Vital signals: These include blood pressure, body temperature, heart rate, and oxygen saturation.
- Patient activity: Includes sleep patterns, movement, and exercise.
Patients can also manually log subjective data such as how they are feeling, alertness, and pain level.
How Are RPM Devices Maintained Or Serviced?
Because the devices are mostly with patients, maintaining and servicing them will require a collaborative approach.
You'll need to train and educate your patients on how to correctly use, maintain, and troubleshoot the devices.
How Long Is RPM Data Stored?
There isn't a standard RPM data storage timeline. Most providers use their own internal policies and guidelines.
Nonetheless, you must abide by state and federal laws and HIPAA requirements.
Conclusion
The benefits of remote patient monitoring are clear. They help enhance the doctor-patient relationships that make superior health outcomes possible.
To ease the process and ensure a successful RPM implementation, KangarooHealth offers services such as device procurement and distribution, training for providers and staff, and patient education and monitoring.
We can help you execute an RPM program that fosters the meaningful connections you need with your patients. Speak with our team today to see how our RPM solutions can help you deliver patient-centered care at scale without disrupting your current workflows.

Sesily Maness
AuthorDigital health marketing professional with over 10 years of experience bridging clinical and wellness spaces by leveraging innovative technologies, behavioral change programs, and strategic digital marketing.